Ulcer
ULCER
What’s an Ulcer and Why Should You Care?
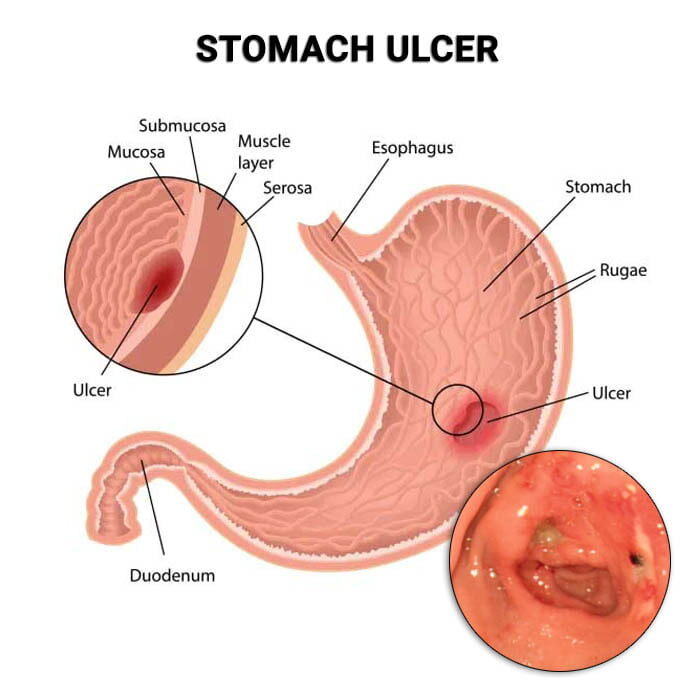
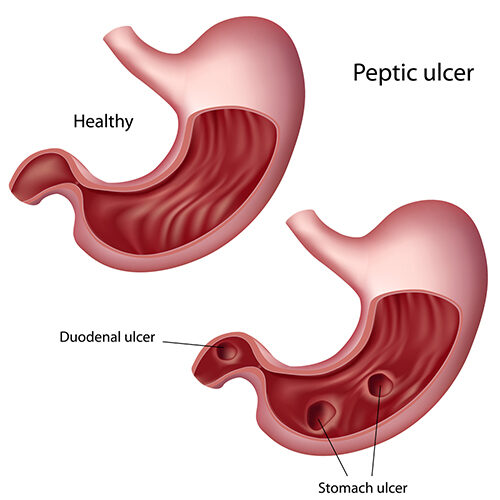
Ever feel a gnawing, burning pain in your stomach? You might be experiencing an ulcer. But what exactly is an ulcer? An ulcer is a sore or lesion that develops on the lining of your esophagus, stomach, or small intestine. They can be incredibly painful and, if left untreated, can lead to serious health complications.
Most people associate ulcers with stress or spicy foods, but the real culprits are often more specific. Understanding the actual causes is the first step toward prevention and treatment.
The Main Causes of Ulcers
It’s a common misconception that lifestyle choices like a high-stress job or a love for hot peppers directly cause ulcers. While these factors can worsen symptoms, the primary causes are usually one of two things:
-
- H. Pylori Bacteria: This is the most common cause of ulcers. Helicobacter pylori is a type of bacteria that lives in the digestive tract. It can weaken the protective mucous lining of the stomach and small intestine, allowing stomach acid to create a sore.
-
- NSAID Use: Frequent or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) is the second leading cause. These over-the-counter pain relievers, like ibuprofen and naproxen, can interfere with the stomach’s ability to protect itself from acid.
Symptoms to Watch For
The symptoms of an ulcer can vary, but here are the most common signs:
-
- Burning Stomach Pain: This is the hallmark symptom. The pain is often felt between your breastbone and navel. It may get worse on an empty stomach and can wake you up at night.
-
- Bloating and Belching: Feeling uncomfortably full after eating, along with frequent burping.
-
- Nausea and Vomiting: A feeling of sickness and, in some cases, throwing up.
-
- Heartburn: A burning sensation in your chest, often rising from your stomach.
In severe cases, an ulcer can lead to vomiting blood or passing black, tarry stools. If you experience these symptoms, seek immediate medical attention, as it could indicate a bleeding ulcer.
Diagnosing an ulcer, particularly a peptic ulcer in the stomach or duodenum, typically begins with a detailed review of the patient’s symptoms and medical history. Doctors will ask about the type and location of pain (often a burning or gnawing sensation in the upper abdomen), its relation to meals, and any history of taking non-steroidal anti-inflammatory drugs (NSAIDs) or family history of ulcers. Since the bacterium Helicobacter pylori (H. pylori) is a primary cause of ulcers, a key part of the diagnostic process is testing for its presence.
The most common diagnostic tests for ulcers and their causes include:
-
Endoscopy (Upper GI Endoscopy): This is considered the “gold standard” for diagnosing an ulcer. A doctor inserts a thin, flexible tube with a camera (an endoscope) down the throat to view the lining of the esophagus, stomach, and duodenum. This allows them to visually identify any ulcers and, if necessary, take a tissue sample (biopsy) to test for H. pylori or rule out cancer.
-
Tests for H. pylori:
-
Breath Test: The patient swallows a special liquid containing a labeled carbon. If H. pylori is present, it breaks down the substance, and the labeled carbon is exhaled in the breath, which is then measured.
-
Stool Antigen Test: A lab tests a stool sample for proteins (H. pylori antigens) from the bacteria.
-
Blood Test: This test checks for antibodies to H. pylori. While it can indicate a past or current infection, it’s generally less accurate than breath or stool tests because antibodies can remain in the blood after the infection is gone.
-
-
Upper GI Series (Barium Swallow): In cases where an endoscopy isn’t feasible, this imaging test can be used. The patient swallows a chalky liquid called barium, which coats the digestive tract and makes it visible on an X-ray, allowing the doctor to see the outline of an ulcer.